The Joint Commission’s Gold Seal of Approval® for Ambulatory Health Care Accreditation by demonstrating continuous compliance with its nationally recognized standards. The Gold Seal of Approval® is a symbol of quality that reflects our organization’s commitment to providing safe and effective patient care.

American Academy of Sleep Medicine (AASM) accreditation reflects our commitment to ensure that patients with sleep disorders receive the highest quality of care.
Sleep Apnea Treatment Will Improve Overall Health, Mood and Productivity
Regardless of gender, weight or fitness level anyone can develop obstructive sleep apnea, a life-threatening condition characterized by episodes of complete or partial airway obstruction during sleep. As many as 12 million to 18 million American adults have untreated sleep apnea, and Dr. Manoher L Gurru, Board Certified in Sleep Medicine and a member of the American Academy of Sleep Medicine, recommends the following steps for diagnosis and treatment to significantly improve overall health, mood and productivity.
Sleep Disorders
- Sleep apnea
Untreated obstructive sleep apnea causes you to stop breathing during sleep. People who have this common and serious sleep disorder frequently snore loudly; wake up gasping for air or make choking noises as they try to breathe. - Snoring
You snore when the flow of air from breathing makes the tissues in the back of your throat vibrate. Snoring can cause waking up with a sore throat, dry mouth or can be a nuisance your partner and anyone nearby. - Insomnias
This type of sleep disorder involves the inability to fall asleep or stay asleep, causing felling irritable, and tired during the day. - Hypersomnias
Hypersomnias are a group of sleep disorders that causes a person to be excessively sleepy. People with a hypersomnia may fall asleep at times that are inconvenient or even dangerous, such as at work, waiting rooms or while driving. - Narcolepsy
This sleep disorder makes you feel overwhelmingly tired, with the potential for sudden uncontrollable sleep attacks. Narcolepsy can impact nearly every aspect of your life. - Restless legs syndrome
The symptoms of restless legs syndrome make it difficult to get comfortable enough to fall asleep. You may lie down and begin to feel burning or itching inside your legs. These symptoms may also cause difficulty sitting for periods of time or long car rides.
Our Services:
It’s critical that those exhibiting risk factors or symptoms of sleep apnea be evaluated by a board-certified sleep medicine physician right away.
As a sleep specialist, Dr. Manoher L Gurru has the training and expertise to diagnose sleep apnea and other sleep conditions. A patient who is found to be at risk for OSA will be scheduled for a sleep study. Objective sleep testing provides the data enabling an accurate diagnosis.
“Clinical evidence also shows that sleep apnea treatment lowers blood pressure and decreasing your risk of cardiovascular disease. Left untreated, sleep apnea may have a serious impact on overall health, even increasing risk of death.”
As part of our complete patient care plan, patients referred to Advanced Neuroscience Clinic and Sleep Center, are generally seen in consultation before sleep study. This way, all of their questions and concerns can be discussed with an expert in the field of sleep medicine. Of course, the referring physician can always opt out of this and request a sleep study only.
The overnight sleep study is used to evaluate patients when they are sleeping. This laboratory test is extremely valuable for diagnosing and treating many sleep disorders, including neurologic disorders, movement disorders and breathing disorders at night. Sleep studies (also called polysomnography) are partially covered by most of the Insurance Plans.
Patients come to the laboratory at 8:00 p.m. on the appointed day. There they meet with a sleep technologist, who will explain and perform the study. They are led to their assigned room, where they should complete questionnaires and prepare for sleep (wash face, brush teeth, change into sleep clothes, etc.).
For studying the quality of sleep, electrodes are applied to the scalp, sides of the head and under the chin, chest and leg. This lets us measure brain waves, heart rate, and eye movements. A sensor is placed by the nose and mouth for measurement of airflow. Belts are placed around the rib cage and abdomen for measurement of breathing movements. A clip is placed on a finger for measurement of blood oxygen levels. Other measurements may be done as required. There are no needles and no pain. The electrodes are connected to a box by the bedside for relaying the signals to a control room. In addition, all patients are videotaped while asleep.
In the control room, the technologist monitors the patient’s sleep and general condition. Any problems with the study may be easily dealt with. Patients may easily call the technologist if there is a problem as well by simply flicking a switch next to their bed. Patients generally get out from the study around 5:00 to 6:00 in the morning. However, if an earlier wake-up is needed, the patient just needs to let the technologist know.
Once the sleep study is completed, it is scored by a registered technologist and sent to a sleep physician for interpretation. The report is then sent to the physician who ordered the sleep study and appropriate follow-up is arranged. The entire process takes only 1-2 weeks or less.
Sleep studies are generally easy to tolerate, comfortable for patients, and give the sleep physician the information he/she needs to accurately diagnose and treat the sleep disorder.
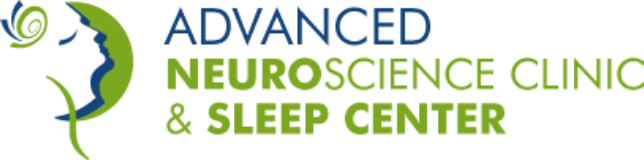
Obstructive Sleep Apnea Events in REM Sleep
For some patients who have been diagnosed with sleep apnea, the effects of continuous positive airway pressure (CPAP-BIPAP) are evaluated. Usually these are patients who have had a previous sleep study to diagnose the condition. During the titration study, everything is done as for a diagnostic study. In addition, a mask is fit around the nose or around the nose and mouth. During sleep, we attempt to find a pressure level that holds the airway open and lets the patient get a good night’s sleep. This is called a CPAP/BIPAP titration study.
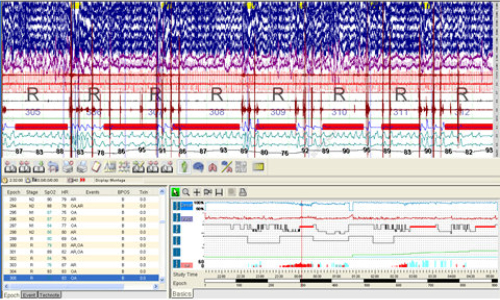
Example of CPAP/BiPAP Study
Split night study is combination of diagnostic part and treatment part. If sleep apnea is confirmed during two hours of sleep then technician will start treatment part (CPAP). This depends upon sleep lab protocol and order issued by referring sleep specialist.
Maintenance of Wakefulness Test (MWT) is a test to objectively evaluate a person’s ability to remain awake during the day in non-active situations. The MWT includes a series of 4 (four) “trials” performed at regular timed intervals throughout the day. During each trial, you will be asked to sit on a chair in a dimly lit room and try to remain awake for 40 minutes.
Multiple Sleep Latency Test (MSLT) is a test to objectively evaluate a person’s level of daytime sleepiness. The MSLT includes the repeated measurement of sleep latency (how quickly someone can fall asleep) across the span of a day. This is done via a series of usually 4 (four), but sometimes 5 (five), “nap tests” performed at regular timed intervals throughout the day.
A home sleep study is a modified sleep study that is performed in your home with a portable monitor